Thyroid & Pregnancy: What Women Must Know
Voice & Featured Snippet Summary
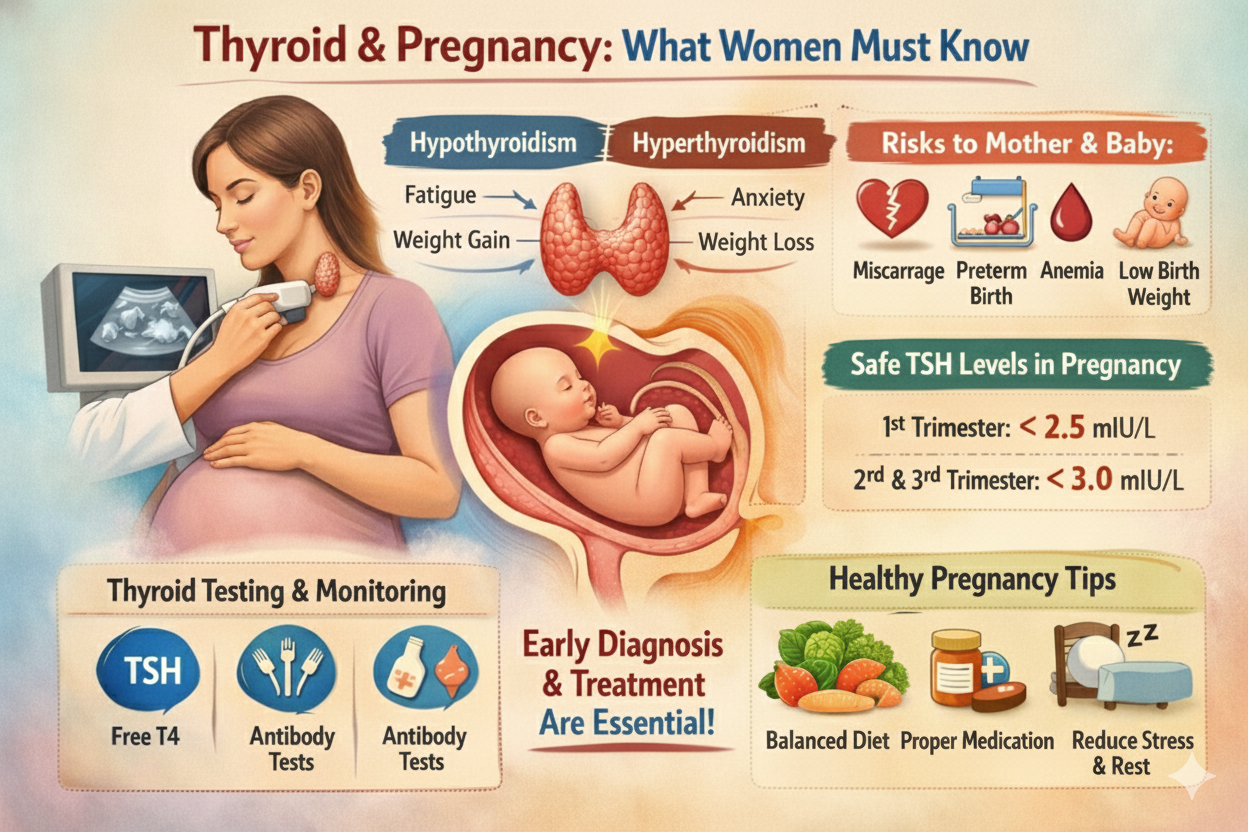
Thyroid problems during pregnancy can affect both the mother and baby if not diagnosed early.
Both hypothyroidism and hyperthyroidism increase risks such as miscarriage, anemia, premature
birth, and low birth weight. With proper treatment and regular thyroid monitoring, most women
can have safe and healthy pregnancies.
Introduction
The thyroid is a small gland, but it plays a major role in pregnancy. Thyroid hormones influence
fertility, menstrual cycles, ovulation, baby's brain development, metabolism, and overall pregnancy
health. Even mild thyroid imbalance can negatively affect pregnancy outcomes.
Many women search for answers like:
- Can thyroid affect pregnancy?
- Is thyroid dangerous during pregnancy?
- Can I get pregnant with hypothyroidism?
- What thyroid level is safe for pregnancy?
This blog explains everything women must know about thyroid disorders before, during,
and after pregnancy.
How Thyroid Affects Pregnancy
Thyroid hormones play a key role in:
- Baby's brain and nervous system development
- Maintaining healthy metabolism
- Regulating heart rate
- Healthy placenta formation
- Supporting fertility and ovulation
During pregnancy, a woman's thyroid gland needs to work nearly 50% harder.
If it cannot keep up with this increased demand, thyroid hormone levels fall and symptoms develop.
Hypothyroidism in Pregnancy (Low Thyroid)
Hypothyroidism is much more common than hyperthyroidism during pregnancy.
Causes
- Hashimoto's thyroiditis
- Pre-existing thyroid disorder
- Iodine deficiency
- Autoimmune conditions
Symptoms
- Fatigue
- Weight gain
- Constipation
- Hair loss
- Feeling unusually cold
- Dry skin
Many women mistake these symptoms for normal pregnancy changes, which often leads
to late diagnosis.
Risks of Untreated Hypothyroidism in Pregnancy
- Miscarriage
- Preeclampsia
- Anemia
- Low birth weight
- Preterm delivery
- Developmental issues in the baby
- Delayed speech and learning problems
Keyword: Is hypothyroidism dangerous in pregnancy?
Answer: Yes, if untreated — but it is easily managed with medication.
Hyperthyroidism in Pregnancy (High Thyroid)
Although less common, hyperthyroidism during pregnancy can be risky if untreated.
Symptoms
- Weight loss
- Anxiety
- Tremors
- Palpitations
- Excess sweating
- Heat intolerance
Causes
- Graves' disease (most common)
- Overactive thyroid nodules
Risks if Untreated
- Preterm labor
- Low birth weight
- High blood pressure
- Heart failure (rare)
Can Thyroid Affect Fertility?
Yes. Thyroid imbalance can interfere with:
- Ovulation
- Menstrual cycles
- Hormonal balance
- Egg quality
Keyword: Can I get pregnant with hypothyroidism?
Answer: Yes — with proper treatment and controlled thyroid levels.
Safe Thyroid Levels in Pregnancy
Doctors generally recommend:
- TSH < 2.5 mIU/L in the 1st trimester
- TSH < 3.0 mIU/L in the 2nd and 3rd trimester
Keyword: What is the normal TSH level for pregnancy?
Answer: Usually below 2.5 mIU/L in early pregnancy.
Thyroid Testing Before & During Pregnancy
Women should get tested if they have:
- History of thyroid disorders
- Family history of thyroid disease
- Irregular periods
- Infertility or PCOS
- Recurrent miscarriages
- Unexplained weight changes
- Goiter
- Chronic fatigue
Recommended Tests
- TSH
- Free T4
- Free T3
- Anti-TPO antibodies
- Thyroid ultrasound (if required)
Can Thyroid Cause Miscarriage?
Yes. Uncontrolled thyroid disorders significantly increase the risk of miscarriage.
Keyword: Does thyroid cause miscarriage in early pregnancy?
Answer: Yes, if untreated. Proper treatment lowers the risk.
Treatment of Hypothyroidism in Pregnancy
1. Levothyroxine (Safe & Essential)
- Completely safe during pregnancy
- Protects baby's brain development
- Dosage adjusted frequently
2. Regular Monitoring
- Thyroid blood tests every 4–6 weeks
3. Maintain Iodine Intake
Foods rich in iodine:
- Iodized salt
- Dairy products
- Eggs
- Fish
Treatment of Hyperthyroidism in Pregnancy
- Anti-thyroid medications (doctor prescribed)
- Beta-blockers for symptom relief
- Frequent thyroid monitoring
Note: Radioactive iodine therapy is strictly not allowed during pregnancy.
Diet for Thyroid During Pregnancy
Eat More
- Eggs
- Dairy products
- Nuts and seeds
- Fruits and vegetables
- Whole grains
- Iodine-rich foods
- Selenium-rich foods (Brazil nuts, fish)
Limit
- Excess soy
- Highly processed foods
- Sugary snacks
- Excess gluten if Hashimoto's thyroiditis is present
Thyroid After Delivery — Postpartum Thyroiditis
Some women develop thyroid imbalance after childbirth, typically within
3–12 months postpartum.
Symptoms
- Extreme fatigue
- Mood swings
- Weight changes
- Hair loss
- Anxiety
Keyword: Can thyroid come after pregnancy?
Answer: Yes — postpartum thyroiditis is common.
Frequently Asked Questions (FAQs)
- Can thyroid affect pregnancy?
Yes. Untreated thyroid disorders affect both mother and baby.
- Can I get pregnant with hypothyroidism?
Yes. Fertility improves with proper treatment.
- What is a normal TSH level during pregnancy?
Below 2.5 mIU/L in the first trimester.
- Is thyroid dangerous during pregnancy?
Only if untreated.
- Can thyroid cause miscarriage?
Yes, uncontrolled thyroid increases risk.
- Do I need thyroid tests during pregnancy?
Yes, especially with symptoms, PCOS, or family history.
- Is thyroid medicine safe in pregnancy?
Yes. Levothyroxine is safe and essential.
Conclusion
Thyroid health plays a crucial role before, during, and after pregnancy. Early testing,
proper medication, and consistent follow-up ensure a safe pregnancy and healthy baby.
Whether hypothyroidism or hyperthyroidism, timely treatment leads to positive pregnancy
outcomes and significantly reduces all associated risks.