- ashish.dr88@gmail.com
- +91-9901312125
- Alexander Rd, Kummari Guda, Shivaji Nagar, Secunderabad, Telangana 500003
INTRODUCTION:
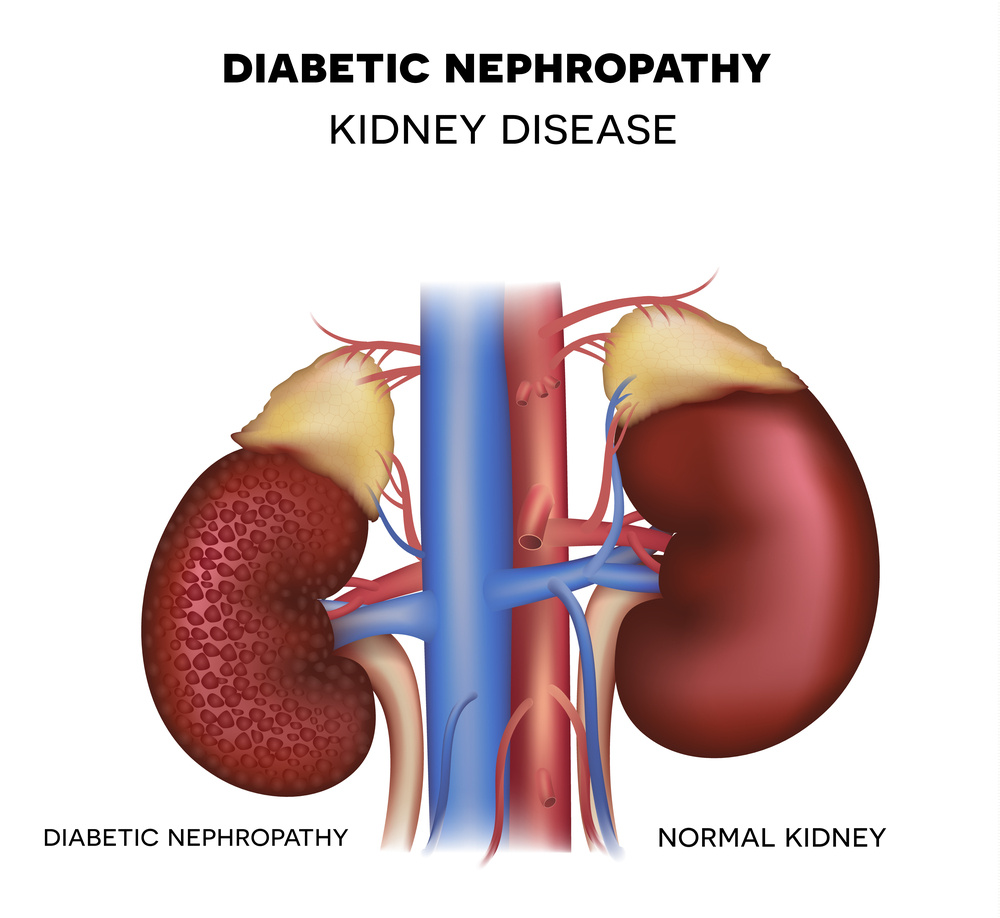
A chronic and irreversible reduction in glomerular filtration (GFR), arterial hypertension, and albuminuria (>300 mg/day or > 200 mcg/min) verified at least twice within three to six months are the characteristics of diabetic nephropathy (DN), a clinical syndrome.
Patients with diabetes who have structural and functional problems in their kidneys are said to have diabetic nephropathy.
The kidney's enlargement, stronger glomerular basement membrane, tubular atrophy, widespread and nodular glomerulosclerosis, and interstitial fibrosis are among the structural abnormalities.
The functional alterations include an early increase in GFR with intraglomerular hypertension,subsequent proteinuria, systemic hypertension, and eventual loss of renal function.
EPIDEMIOLOGY:
Diabetic nephropathy is a major cause of morbidity and mortality for persons with either T1DM or T2DM. Globally, diabetes is the primary cause of end-stage renal disease.Diabetic kidney damage eventually develops in 5% to 40% of patients with type 2 diabetes and 25% to 40% of patients with type 1 diabetes.
Up to 20% of T2DM patients are diagnosed with diabetic kidney disease, and another 30% to 40% go on to develop diabetic nephropathy, typically within ten years of their diagnosis. Over 80% of diabetic patients receiving renal replacement treatment have T2DM, despite the fact that nephropathy seems to be more common in T1DM due to the huge and growing number of people with T2DM.
NATURAL HISTORY OF DN:
Diabetic nephropathy is characterized clinically as a triad of hypertension, proteinuria, and, renal impairment.
Even
though natural history of diabetic nephropathy has been better described in
Type 1 DM, the classification by Mogensen into five stages of nephropathy, can
be applied to both forms of diabetes.
Mogensen classification of diabetic nephropathy:
Stage 1:Hyperfiltration
Stage
2:Silent stage-normal albuminurias
Stage
3:Incipient stage-microalbuminuria
Stage
4:Overt stage-macroalbuminuria
Stage
5:End stage renal disease
·
DN,diabetic nephropathy;ESRD,end
stage renal disease;GFR,glomerular filtration rate;UAE,urinary albumin
excretion.
· Pugliese G Acta
Diabetol 2014;51:905-915
STAGE
1 HYPERFILTRATION:
When Type I DM is
diagnosed, this stage is observed. At this point, renal vasodilatation and
hyperfiltration take place. There is an increase in glomerular filtration rate
(GFR) in 41% of Type 2 DM and 90–“95% of Type 1 DM. The primary reasons of
elevated GFR are decreased plasma oncotic pressure and elevated renal plasma
flow (RPF). But for any given RPF, GFR is higher. In diabetics, this is a sign
of elevated glomerular capillary hydrostatic pressure.
STAGE 2 SILENT STAGE:
Patients'
urine albumin excretion (UAE) is still between 15 and 20 micrograms per minute
at this stage. Exercise can lead to temporary microalbuminuria, which returns
to normal at rest.
Blood pressure is either normal or slightly increased, and the glomerular filtration rate is often high. Patients with type 2 diabetes who have microalbuminuria exhibit elevated glomerular volume, indicating that microalbuminuria is a sign of diabetic kidney damage regardless of GFR.
STAGE 3 INCIPIENT DIABETIC NEPHROPATHY MICROALBUMINURIA:
In this stage, the UAE is between 20-200 mg/min or 30-300 mg/24 hr. Patients with microalbuminuria have negative urine dipstick for protein and less than 300 mg in 24 hours. This stage occurs usually 5 to 15 years after diagnosis of diabetes.
In
patients with Type 1 DM, microalbuminuria is a risk factor for progression to
nephropathy. In patients with Type 2 DM ,it is less predictive because of
comorbid conditions which are associated with microalbuminuria and death may occur
before development of nephropathy. Microalbuminuria is also associated with
increased risk of cardiovascular death in both forms of diabetes.
STAGE 4 OVERT DIABETIC NEPHROPATHY-MACROALBUMINURIA:
This stage is defined by onset of clinical proteinuria, i.e. persistent dipstick positive albuminuria (UAE > 300mg/ day or urinary protein excretion of more than 500mg/day). It usually occurs 15-20 years after onset of Type 1 DM and after 10-12 years of Type 2 DM.
In association with this increase in proteinuria, more than two thirds of patients have overt systemic hypertension. During this phase, if left untreated, BP continues to rise, accelerating the decline in GFR, which promotes a further rise in BP, creating a vicious cycle of progressive renal impairment that ultimately leads to ESRD.
STAGE 5 END STAGE RENAL DISEASE:
Very low GFR and widespread glomerular sclerosis are characteristics of this stage. Complications including edema and fluid retention are linked to the development of uremia.
Since kidney transplantation is linked to better results than continuing dialysis, many people with diabetes and end-stage renal disease are now seen as potential candidates.
RISK
FACTORS FOR DIABETIC NEPHROPATHY:
SCREENING AND DIAGNOSIS:
Screening for microalbuminuria is recommended for
type 2 diabetics from the day of diagnosis on annual basis, while in type 1
diabetics, annual screening should be done after 5 years of diagnosis of type 1
DM.
Screening can be
performed by measurement of albumin to creatinine ratio in the random spot
urine sample or 24 hour or timed urine collections which are more burdensome
and add little to prediction or accuracy.
Because of
variability in urine albumin excretion rate (UAE), two of the three specimens
collected consecutively should be abnormal.
A 24 hour
urinary collection is gold standard for detection of microalbuminuria.
Screening for microalbuminuria
ABNORMALITIES IN
ALBUMIN EXCRETION
Screening should not be performed in the presence of conditions that increase UAE, such as urinary tract infection, hematuria, acute febrile illness, vigorous exercise, short-term pronounced hyperglycemia, uncontrolled hypertension,
and heart
failure.
Serum creatinine should be measured at baseline and annually in all diabetics,regardless of UAE rate.
Estimated GFR(eGFR ) is usually calculated by the –modification of diet in renal disease(MDRD) study– equation.
MDRD study equation:
GFR(mL/min/1.73
m2 )=175Á—(Scr)-1.154 Á— (Age) -0.203 Á— (0.742
if female)Á—(1.212 if African –“american)
Based on eGFR ,chronic kidney disease (CKD) is graded into five stages(G1 to G5).In combination with degree of albuminuria (A1,A2,A3),CKD stages are classified into various risk categories for progression of CKD.
TREATMENT
OF END STAGE RENAL DISEASE:
The renal replacement
modalities available for patients with ESRD from diabetes include peritoneal dialysis,
hemodialysis, and renal transplantation.
Diabetic patients with autonomic dysfunction or diastolic dysfunction are more often likely to develop hypotension during hemodialysis due to poor toleration of volume shifts. Due to gradual fluid removal in continuous ambulatory peritoneal dialysis, the procedure is not usually associated with hypotension unless the patient is volume-depleted,and it is thus better suited for patients with diabetes.
Peripheral
vascular disease is common in older patients with type-2 diabetes and this
limits the ability to create and sustain adequate vascular access for HD.
Mortality and morbidity are substantially higher in patients with diabetes maintained on dialysis than in their nondiabetic counterparts with cardiovascular disease and infections being the leading causes of death.
Renal transplantation is associated with better survival, improved quality of life, and a higher degree of rehabilitation compared to dialysis.
Recurrence of DN
can occur in the allografts. This occurs as a result of poor glycemic control
and/or insulin deficiency. Offering the patient with type-I diabetes combined
pancreas-kidney transplantation can prevent
recurrence of DN.
PREVENTION
OF DN:
Primary prevention:
The goal of primary prevention is to keep people from developing diabetes.
Weight control
and regular exercise are two lifestyle changes that have been demonstrated to
either prevent or postpone the onset of diabetes.
Additionally,
exercise improves insulin sensitivity and blood cholesterol levels, lowers
blood pressure, increases endothelial health, and decreases the proportion of
total and belly fat.
The left
ventricle's diastolic and vasodilator functions.
It has also been
shown that pharmacologic therapies involving glucose-lowering medications in
high-risk individuals significantly reduce the incidence of diabetes.
However,
medication therapy was less effective and linked to serious negative side
effects when compared to lifestyle approaches.
Secondary
prevention:
Strict
management of blood pressure, cholesterol, and blood sugar levels is part of
secondary prevention. Proteinuria screening and the implementation of suitable
treatment constitute tertiary prevention.
References:
1. Reeves WB,
Andreoli TE. Transforming growth factor b contributes to progressive diabetic
nephropathy. Proc NatI Acad Sci USA. 2000;97:7667-7669.
2. Alebiosu CO,
Kadiri S, Akang EEU. Clinicopathological study of Diabetic
Nephropathy
based on Renal Biopsy. Diabetes Intemational. 2002;12:66-69.
3. Kimmestiel P,
Wilson C. Intercapillary lesions in the glomeruli of the kidney.
Am J Path.
1936;1 2:83-97.
4. Hostetter TH,
Troy JL, Brenner BM. Glomerular hemodynamics in experimental
diabetes. Kidney
Int. 1981;19:410-415.
5. Hostetter TH,
Rennke GH, Brenner BM. The case for intrarenal hypertension
in the
initiation and progression of diabetic and other glomerulopathies.
Am J Med. 1982;72:375-380.
6: Gilbertson DT, Liu J, Xue JL, et al.
Projecting the number of patients with end-stage renal disease in the United
States to the year 2015.J Am Soc Nephrol. 2005;16:3736-3741.
7:Ismail N, Becker B, Strzelczyk P, et
al. Renal disease and hypertensionin non–“insulin-dependent diabetes mellitus. Kidney
Int. 1999;55:1-28.
8: Parving HH,
Hommel E, Mathiesen E, et al. Prevalence of microalbuminuria,
arterial hypertension,
retinopathy and neuropathy in
patients with
insulin dependent diabetes. Br Med J (Clin Res Ed).
1988;296:156-160.
9. Standl E,
Stiegler H. Microalbuminuria in a random cohort of recently
diagnosed type 2
(non–“insulin-dependent) diabetic patients living in
the greater
Munich area. Diabetologia. 1993;36:1017-1020.
10. Schmitz A,
Vaeth M, Mogensen CE. Systolic blood pressure relates to
the rate of
progression of albuminuria in NIDDM. Diabetologia.
1994;37:1251-1258.
11: Zimmet P,
Alberti KG, Shaw J. Global and societal implications of the
diabetes
epidemic. Nature. 2001;414:782-787.
12: Mogensen
CE, Christensen CK, Vittinghus E. The stages in diabetic renal disease. With
emphasis in the stage of incipient diabetic nephropathy. Diabetes.
1983;32(Suppl 2):64-78.
13: Cooper ME.
Pathogenesis, prevention, and treatment of diabetic nephropathy. Lancet 1998;
352: 213–“219.
14: Cooper ME.
Interaction of metabolic and haemodynamic factors in mediating experimental
diabetic nephropathy.Diabetologia 2001; 44: 1957–“1972.
15: American
Diabetes Association: Nephropathy in diabetes (Position Statement).
Diabetes Care 27
(Suppl.1):S79–“S83, 2004.
16: Prakash
J, Sen D, Usha, Kumar NS. Non–'diabetic renal disease in patients with type 2
Diabetes mellitus. J Assoc Physicians India 2001;49:415–'20.
17: Mulec
H, Blohme G, Grandi B, et al. The effect of metabolic control on
rate of decline
in renal function in insulin-dependent diabetes mellitus with
overt diabetic
nephropathy. Nephrol Dial Tronspoant. 1998;13:651-655.
18: Standards
of medical care for patients with diabetes mellitus (Position
Statement).
Clinical Practice Recommendations 2001. Diabetes Care.2001 ;24 (suppli
):S33-S43.
19: Bakris
GL, Williams M, Dworkin L, et al. Preserving renal function in adults
with
hypertension and diabetes: a consensus approach. Am J Kidney Dis.
2000;36:646-66
1.
20: American
Diabetes Association. Treatment of hypertension in adults
with diabetes.
Diabetes Care. 2003;26(Suppl 1 ):S80-S82.
21: NKF-K/DOQI
Clinical Practice Guidelines for Nutrition in Chronic Renal
Failure. Am J
Kidney Dis. 2002;35:S1-S140.
22: Lam
KSL, Cheing IKP, Jamis ED, et al. Cholesterol-lowering therapy may
retard the
progression of diabetic nephropathy. Diabetologia. 1995;38:604-609.
23: Fried LF,
Orchard TJ, Kasiske BL. The effect of lipid reduction on renal disease
progression. A meta-analysis. Kidney Int. 2001;59:260-269.
24:
Hans-Henrik Parving.,
Frederik Persson, et al.Aliskiren Combined with Losartan in Type 2
Diabetes and Nephropathy:N Engl J Med 2008; 358:2433-2446
25: Murray
Epstein et al. Selective Aldosterone Blockade with Eplerenone Reduces
Albuminuria in Patients with Type 2 Diabetes: Clin J Am Soc Nephrol 1: 940–“951,
2006.
26: Bakris
G, Viberti G, Weston WM, et al. Rosiglitazone reduces urinary
albumin
excretion in type-2 diabetes. J Human Hypertens. 2003;17:7-12.
27:Pablo E Pargola et
al.
Bardoxolone
Methyl and Kidney Function in CKD with Type 2 Diabetes: N Engl J Med 2011; 365:327-336.
28: Johannes F.E. Mann, et al.Avosentan for Overt Diabetic Nephropathy:
J Am Soc Nephrol. 2010 Mar; 21(3):
527–“535.